Palpitations
| Palpitation | |
|---|---|
 | |
| Artistic impression of a woman experiencing syncope, which may accompany heart palpitations | |
| Specialty | Cardiology |
| Differential diagnosis | Tachycardia |
Palpitations occur when a person becomes aware of their heartbeat. The heartbeat may feel hard, fast, or uneven in their chest. [1]
Symptoms include a very fast or irregular heartbeat. Palpitations are a sensory symptom. [1]They are often described as a skipped beat, a rapid flutter, or a pounding in the chest or neck. [1]
Palpitations are not always the result of a physical problem with the heart and can be linked to anxiety. However, they may signal a fast or irregular heartbeat. Palpitations can be brief or long-lasting. They can be intermittent or continuous. Other symptoms can include dizziness, shortness of breath, sweating, headaches, and chest pain.
Palpitation may be associated with coronary heart disease, perimenopause, hyperthyroidism, heart muscle diseases like hypertrophic cardiomyopathy, diseases causing low blood oxygen such as asthma, emphysema or a blood clot in the lungs; previous chest surgery; kidney disease; blood loss and pain; anemia; drugs such as antidepressants, statins, alcohol, nicotine, caffeine, cocaine and amphetamines; electrolyte imbalances of magnesium, potassium and calcium; and deficiencies of nutrients such as taurine, arginine, iron or vitamin B12.[2]
Signs and symptoms
[edit]Three common descriptions of palpitation are:
- "flip-flopping" (or "stop and start") is often caused by premature contraction of the atrium or ventricle. The pause after the contraction causes the "stop." The "start" comes from the next forceful contraction.
- rapid "fluttering in the chest" suggests arrhythmias. Regular "fluttering" points to supraventricular or ventricular arrhythmias, including sinus tachycardia. Irregular "fluttering" suggests atrial fibrillation, atrial flutter, or tachycardia with variable block.
- "pounding in the neck" or neck pulsations, often due to cannon A waves in the jugular vein. These occur when the right atriumcontracts against a closed tricuspid valve.[3]
Palpitation associated with chest pain suggests coronary artery disease, or if the chest pain is relieved by leaning forward, pericardial disease is suspected. Palpitation associated with light-headedness, fainting or near fainting suggest low blood pressure and may signify a life-threatening cardiac dysrhythmia. Palpitation that occurs regularly with exertion suggests a rate-dependent bypass tract or hypertrophic cardiomyopathy.
If a benign cause for these symptoms isn't found at the first visit, then prolonged heart monitoring at home or in the hospital setting may be needed. Noncardiac symptoms should also be elicited since the palpitations may be caused by a normal heart responding to a metabolic or inflammatory condition. Weight loss suggests hyperthyroidism. Palpitation can be precipitated by vomiting or diarrhea that leads to electrolyte disorders and hypovolemia. Hyperventilation, hand tingling, and nervousness are common when anxiety or panic disorder is the cause of the palpitations.[4]
Causes
[edit]The responsibility for the perception of heartbeat by neural pathways is not clear. It has been hypothesized that these pathways include different structures located both at the intra-cardiac and extra-cardiac level.[1] Palpitations are a widely diffuse complaint and particularly in subjects affected by structural heart disease.[1] The list of causes of palpitations is long, and in some cases, the etiology is unable to be determined.[1] In one study reporting the etiology of palpitations, 43% were found to be cardiac, 31% psychiatric, and approximately 10% were classified as miscellaneous (medication induced, thyrotoxicosis, caffeine, cocaine, anemia, amphetamine, mastocytosis).[1]
The cardiac etiologies of palpitations are the most life-threatening and include ventricular sources (premature ventricular contractions (PVC), ventricular tachycardia and ventricular fibrillation), atrial sources (atrial fibrillation, atrial flutter) high output states (anemia, AV fistula, Paget's disease of bone or pregnancy), structural abnormalities (congenital heart disease, cardiomegaly, aortic aneurysm, or acute left ventricular failure), and miscellaneous sources (postural orthostatic tachycardia syndrome abbreviated as POTS, Brugada syndrome, and sinus tachycardia).[1]
Palpitation can be attributed to one of five main causes:
- Extra-cardiac stimulation of the sympathetic nervous system (inappropriate stimulation of the sympathetic and parasympathetic, particularly the vagus nerve, (which innervates the heart), can be caused by anxiety and stress due to acute or chronic elevations in glucocorticoids and catecholamines.[1] Gastrointestinal distress such as bloating or indigestion, along with muscular imbalances and poor posture, can also irritate the vagus nerve causing palpitations)
- Sympathetic overdrive (panic disorder, low blood sugar, hypoxia, antihistamines (levocetirizine), low red blood cell count, heart failure, mitral valve prolapse).[5]
- Hyperdynamic circulation (valvular incompetence, thyrotoxicosis, hypercapnia, high body temperature, low red blood cell count, pregnancy).
- Abnormal heart rhythms (ectopic beat, premature atrial contraction, junctional escape beat, premature ventricular contraction, atrial fibrillation, supraventricular tachycardia, ventricular tachycardia, ventricular fibrillation, heart block).
- Pectus Excavatum, also known as funnel chest, is a chest wall deformity. When the breastbone (sternum) and attached ribs are sunken in enough to put excess pressure on the heart and lungs which can cause tachycardia and skipped beats.
Palpitations can occur during times of catecholamine excess, such as during exercise or at times of stress.[1] The cause of the palpitations during these conditions is often a sustained supraventricular tachycardia or ventricular tachyarrhythmia.[1] Supraventricular tachycardias can also be induced at the termination of exercise when the withdrawal of catecholamines is coupled with a surge in the vagal tone.[1] Palpitations secondary to catecholamine excess may also occur during emotionally startling experiences, especially in patients with a long QT syndrome.[1]
Psychiatric problems
[edit]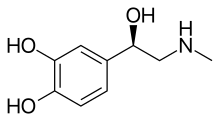
Anxiety and stress elevate the body's level of cortisol and adrenaline, which in turn can interfere with the normal functioning of the parasympathetic nervous system resulting in overstimulation of the vagus nerve. Vagus nerve induced palpitation is felt as a thud, a hollow fluttery sensation, or a skipped beat, depending on at what point during the heart's normal rhythm the vagus nerve fires. In many cases, the anxiety and panic of experiencing palpitations cause a patient to experience further anxiety and increased vagus nerve stimulation. The link between anxiety and palpitation may also explain why many panic attacks involve an impending sense of cardiac arrest. Similarly, physical and mental stress may contribute to the occurrence of palpitation, possibly due to the depletion of certain micronutrients involved in maintaining healthy psychological and physiological function.[6] Gastrointestinal bloating, indigestion and hiccups have also been associated with overstimulation of the vagus nerve causing palpitations, due to branches of the vagus nerve innervating the GI tract, diaphragm, and lungs.[citation needed]
Many psychiatric conditions can result in palpitations including depression, generalized anxiety disorder, panic attacks, and somatization. However one study noted that up to 67% of patients diagnosed with a mental health condition had an underlying arrhythmia.[1] There are many metabolic conditions that can result in palpitations including, hyperthyroidism, hypoglycemia, hypocalcemia, hyperkalemia, hypokalemia, hypermagnesemia, hypomagnesemia, and pheochromocytoma.[1]
Medication
[edit]The medications most likely to result in palpitations include sympathomimetic agents, anticholinergic drugs, vasodilators and withdrawal from beta blockers.[1][7]
Common etiologies also include excess caffeine, or marijuana.[1] Cocaine, amphetamines, 3-4 methylenedioxymethamphetamine (Ecstasy or MDMA) can also cause palpitations.[1]
Pathophysiology
[edit]The sensation of palpitations can arise from extra-systoles or tachyarrhythmia.[1] It is very rarely noted due to bradycardia.[1] Palpitations can be described in many ways.[1] The most common descriptions include a flip-flopping in the chest, a rapid fluttering in the chest, or pounding in the neck.[1] The description of the symptoms may provide a clue regarding the etiology of the palpitations, and the pathophysiology of each of these descriptions is thought to be different.[1] In patients who describe the palpitations as a brief flip-flopping in the chest, the palpitations are thought to be caused by extra- systoles such as supraventricular or ventricular premature contractions.[1] The flip-flop sensation is thought to result from the forceful contraction following the pause, and the sensation that the heart is stopped results from the pause.[1] The sensation of rapid fluttering in the chest is thought to result from a sustained ventricular or supraventricular arrhythmia.[1] Furthermore, the sudden cessation of this arrhythmia can suggest paroxysmal supraventricular tachycardia.[1] This is further supported if the patient can stop the palpitations by using Valsalva maneuvers.[1] The rhythm of the palpitations may indicate the etiology of the palpitations (irregular palpitations indicate atrial fibrillation as a source of the palpitations).[1] An irregular pounding sensation in the neck can be caused by the dissociation of mitral valve and tricuspid valve, and the subsequent atria are contracting against a closed tricuspid and mitral valves, thereby producing cannon A waves.[1] Palpitations induced by exercise could be suggestive of cardiomyopathy, ischemia or channelopathies.[1]
Diagnosis
[edit]To diagnose palpitations, understand how the person describes them. Key details are the age of first noticing the palpitations and the situations in which they occur. It’s also helpful to know about their caffeine intake. Information such as how much coffee or tea they drink. Learning if deep breathing or changing positions can stop the palpitations. It's also important to know how the palpitations start and stop. Do they begin and end suddenly or gradually? Does the heartbeat feel regular or irregular? How fast does the pulse get during an episode? If the person has found a way to stop the palpitations, that’s useful information.[1]
To figure out what’s causing palpitations, a complete history and physical exam are essential.[1] The history should include details like the age when symptoms began, a description of the symptoms (such as the rhythm), and triggers. It should note how quickly they start, how long they last, and what helps (like resting or the Valsalva maneuver). Also, note if certain positions affect the symptoms. Are there other symptoms, like chest pain, dizziness, or fainting? If the person isn’t having palpitations during the visit, they can tap out the rhythm to demonstrate it.
The patient should be asked about all medications, including over-the-counter drugs. Also, ask about their social habits, like exercise, caffeine or alcohol use, and any drug use. Their medical history and family history might also offer clues about the cause of the palpitations.[1]
Palpitations that start in childhood are often caused by supraventricular tachycardia (SVT). Palpitations that appear later in life are more likely linked to structural heart problems.[1] A rapid, regular heartbeat is usually due to paroxysmal SVT or ventricular tachycardia.[1] A rapid, irregular rhythm might be due to atrial fibrillation, atrial flutter, or tachycardia with a variable block.[1] Supraventricular and ventricular tachycardias often cause sudden palpitations. They start and stop quickly. If someone can stop their palpitations with the Valsalva maneuver it may indicate SVT.[1] Palpitations with chest pain could mean reduced blood flow to the heart. If the person feels lightheaded or faints, arrhythmias should be considered.[1]
Diagnosing palpitations can be tricky because it’s rare for symptoms to occur during a routine medical exam or while having an ECG. However, if a heart murmur or abnormal ECG is found, it can provide important clues. Specific changes in the ECG can reveal heart rhythm problems, so a thorough physical exam and ECG are essential.[1]
The physical exam should include checking vital signs and a position based blood pressure. Listening to the heart and lungs and examining the arms and legs for any issues is also important. If the person isn’t having symptoms during the exam, they can tap out the rhythm to show what their heartbeat felt like.[1]
Positive orthostatic vital signs may indicate dehydration or an electrolyte abnormality.[1] A mid-systolic click and heart murmur may indicate mitral valve prolapse.[1] A harsh holo-systolic murmur best heard at the left sternal border which increases with Valsalva may indicate hypertrophic obstructive cardiomyopathy.[1] An irregular rhythm indicates atrial fibrillation or atrial flutter.[1] Evidence of cardiomegaly and peripheral edema may indicate heart failure and ischemia or a valvular abnormality.[1]
Blood tests, especially thyroid function tests, are key baseline tests. An overactive thyroid can cause palpitations. In that case, the thyroid is treated.[8]

The next step in diagnosing palpitations is often 24-hour or longer ECG monitoring using a Holter monitor. This device records the heart's electrical activity nonstop for 24 to 48 hours. If symptoms happen during this time, doctors can check the recording to see what the heart rhythm looked like. However, for this test to work well, the symptoms need to occur at least once a day. If symptoms are less frequent, the chances of finding anything with 24- or 48-hour monitoring go down. Newer technology, like the Zio Patch, allows for continuous heart monitoring for up to 14 days. Patients press a button on the patch when symptoms occur and keep a log of the events.[9]
Other types of monitoring can be helpful if symptoms happen less often. A continuous-loop event recorder constantly monitors the heart. It only saves the data when the patient activates it. When activated, it records the heart's activity for a set time before and after. A cardiologist can adjust this time. For people with rare but severe symptoms, an implantable loop recorder may be useful. This small device is placed under the skin on the chest, similar to a pacemaker. It uses a radio signal to communicate with an external device. It can store information for doctors to analyze.
Sometimes, checking the heart's structure is also important. Most people with palpitations have a normal heart. But, there may be issues, like valve problems, in some cases. In these cases, a doctor may hear a murmur and perform an ultrasound of the heart, called an echocardiogram. This test uses sound waves to create images of the heart. It is painless, like the ultrasounds used to check a baby during pregnancy.
Evaluation
[edit]A 12-lead electrocardiogram must be performed on every patient complaining of palpitations.[1] The presence of a short PR interval and a delta wave (Wolff-Parkinson-White syndrome) is an indication of the existence of ventricular pre-excitation.[1] Significant left ventricular hypertrophy with deep septal Q waves in I, L, and V4 through V6 may indicate hypertrophic obstructive cardiomyopathy.[1] The presence of Q waves may indicate a prior myocardial infarction as the etiology of the palpitations, and a prolonged QT interval may indicate the presence of the long QT syndrome.[1]
Laboratory studies should be limited initially.[1] Complete blood count can assess for anemia and infection.[1] Serum urea, creatinine and electrolytes to assess for electrolyte imbalances and renal dysfunction.[1] Thyroid function tests may demonstrate a hyperthyroid state.[1]
Most patients have benign conditions as the etiology for their palpitations.[1] The goal of further evaluation is to identify those patients who are at high risk for an arrhythmia.[1] Recommended laboratory studies include an investigation for anemia, hyperthyroidism and electrolyte abnormalities.[1] Echocardiograms are indicated for patients in whom structural heart disease is a concern.[1]
Further diagnostic testing is recommended for those in whom the initial diagnostic evaluation (history, physical examination, and EKG) suggest an arrhythmia, those who are at high risk for an arrhythmia, and those who remain anxious to have a specific explanation of their symptoms.[1] People considered to be at high risk for an arrhythmia include those with organic heart disease or any myocardial abnormality that may lead to serious arrhythmias.[1] These conditions include a scar from myocardial infarction, idiopathic dilated cardiomyopathy, clinically significant valvular regurgitant, or stenotic lesions and hypertrophic cardiomyopathies.[1]
An aggressive diagnostic approach is recommended for those at high risk and can include ambulatory monitoring or electrophysiologic studies.[1] There are three types of ambulatory EKG monitoring devices: Holter monitor, continuous-loop event recorder, and an implantable loop recorder.[1]
People who are going to have these devices checked should be made aware of the properties of the devices and the accompanying course of the examination for each device.[1] The Holter monitor is a 24-hour monitoring system that is worn by exam takers themselves and records and continuously saves data.[1] Holter monitors are typically worn for a few days.[1] The continuous-loop event recorders are also worn by the exam taker and continuously record data, but the data is saved only when someone manually activates the monitor.[1] The continuous-loop recorders can be long worn for longer periods of time than the Holter monitors and therefore have been proven to be more cost-effective and efficacious than Holter monitors.[1] Also, because the person triggers the device when he/she feel the symptoms, they are more likely to record data during palpitations.[1] An implantable loop recorder is a device that is placed subcutaneously and continuously monitors for cardiac arrhythmias.[1] These are most often used in those with unexplained syncope and can be used for longer periods of time than the continuous loop event recorders. An implantable loop recorder is a device that is placed subcutaneously and continuously monitors for the detection of cardiac arrhythmias.[1] These are most often used in those with unexplained syncope and are a used for longer periods of time than the continuous loop event recorders.[1] Electrophysiology testing enables a detailed analysis of the underlying mechanism of the cardiac arrhythmia as well as the site of origin.[1] EPS studies are usually indicated in those with a high pretest likelihood of a serious arrhythmia.[1] The level of evidence for evaluation techniques is based upon consensus expert opinion.[1]
Treatment
[edit]Non-medical treatments
[edit]The patient should avoid anything that brings on palpitations. Stress and anxiety-reducing techniques, like meditation or massage, can help. They can ease symptoms, but only for a short time.
If the palpitations are a temporary rise in heart rate, and the patient is stable, simple techniques called vagal maneuvers might work.[10] They involve slowing the heart rate through certain actions. Changing positions, like sitting up instead of lying down, may help.
If an ongoing issue causes the palpitations, they may return unless medically treated.
Medical treatments
[edit]Treating palpitations depends on how bad they are and what’s causing them.[1]
Radiofrequency ablation is a common treatment for most supraventricular and ventricular tachycardias.[1] Another option is stereotactic radioablation.[1] It was originally performed for tumors. But, it has also treated tough heart rhythm problems. These include ventricular tachycardia and atrial fibrillation.[1]
Some palpitations are caused by extra heartbeats or occur with a normal heart rhythm. These include beats that start above the ventricles or ventricular ectopic beats.[1] These are usually harmless, and patients can be reassured that they’re not dangerous. If the symptoms are bothersome or impact daily life, beta-blockers might help. They can also protect healthy people.[1]
People with no symptoms, normal lab tests, and normal EKG results can usually leave the emergency department safely. They should follow up with their primary care doctor or a cardiologist.[1] However, patients with palpitations linked to fainting (syncope), uncontrolled arrhythmias, poor blood flow (hemodynamic issues), or chest pain (angina) should get further evaluation.[1]
If palpitations are due to heart muscle problems, a cardiologist must be involved in the patient's care.
Palpitations from vagus nerve stimulation are usually not due to heart problems. These types of palpitations originate outside the heart and are not a sign of an unhealthy heart muscle. To treat this type of palpitation, the cause of irritation to the vagus nerve or parasympathetic nervous system needs to be found and fixed. Anxiety and stress can worsen vagus nerve-induced palpitations. So, managing stress is key to treatment.
Prognosis
[edit]Heart rate monitoring with smartphones and smartwatches has become very common. These devices are getting better at detecting heart problems like atrial fibrillation early.[1]
Many people worry when they feel palpitations.[1] However, in most cases, the cause of palpitations is harmless, so detailed medical tests are often not needed.[1] Following up with a primary care doctor can help track symptoms and decide if a heart specialist (cardiologist) is needed.
If someone is at high risk of having a serious heart problem, they may need more testing and treatment. Once the cause of palpitations is found, effective treatments exist. They are backed by good medical research.[1] Working closely with patients to make treatment decisions and involving a healthcare team including nurses,nurse practitioners, physician assistants, and doctors can help ensure the best care and follow-up.[1]
Prevalence
[edit]Palpitations are a common complaint in the general population, particularly in those affected by structural heart disease.[1] Clinical presentation is divided into four groups: extra-systolic, tachycardic, anxiety-related, and intense.[1] Anxiety-related is the most common.[1]
See also
[edit]References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq br bs bt bu bv bw bx by bz ca cb cc cd ce cf cg ch ci cj ck cl cm Robinson, Kenneth J.; Sanchack, Kristian E. (2019). Palpitations in StatPearls. StatPearls. PMID 28613787. Retrieved 2019-03-30 – via NCBI Bookshelf.
 This source from PubMed is licensed under the Creative Commons Attribution 4.0 International License.
This source from PubMed is licensed under the Creative Commons Attribution 4.0 International License.
- ^ "Vitamins That Can Cause Heart Palpitations". LiveStrong. com. Retrieved 2021-09-04.
- ^ Indik, Julia H. (2010). "When Palpitations Worsen". The American Journal of Medicine. 123 (6): 517–519. doi:10.1016/j.amjmed.2010.01.012. PMID 20569756.
- ^ Jamshed, N; Dubin, J; Eldadah, Z (February 2013). "Emergency management of palpitations in the elderly: epidemiology, diagnostic approaches, and therapeutic options". Clinics in Geriatric Medicine. 29 (1): 205–230. doi:10.1016/j.cger.2012.10.003. PMID 23177608.
- ^ MedlinePlus Medical Encyclopedia: Heart palpitations
- ^ Cernak, I; Savic, V; Kotur, J; Prokic, V; Kuljic, B; Grbovic, D; Veljovic, M (2000). "Alterations in magnesium and oxidative status during chronic emotional stress". Magnesium Research. 13 (1): 29–36. PMID 10761188.
- ^ Weitz, HH; Weinstock, PJ (1995). "Approach to the patient with palpitations". The Medical Clinics of North America. 79 (2): 449–456. doi:10.1016/S0025-7125(16)30078-5. ISSN 0025-7125. PMID 7877401.
- ^ Debmalya, Sanyal; Saumitra, Ray; Singh, Malhi Harshveer (2022-10-01). "Interplay between cardiovascular and thyroid dysfunctions: A review of clinical implications and management strategies". Endocrine Regulations. 56 (4): 311–328. doi:10.2478/enr-2022-0033. PMID 36270343. S2CID 253046152.
- ^ "Zio XT Subject Instructions & Button Press Log" (PDF). MESA. University of Washington Collaborative Health Studies Coordinating Center. Retrieved 13 December 2024.
- ^ Page, Richard L.; Joglar, José A.; Caldwell, Mary A.; Calkins, Hugh; Conti, Jamie B.; Deal, Barbara J.; Estes, N.A. Mark; Field, Michael E.; Goldberger, Zachary D.; Hammill, Stephen C.; Indik, Julia H.; Lindsay, Bruce D.; Olshansky, Brian; Russo, Andrea M.; Shen, Win-Kuang (2016-04-05). "2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society". Circulation. 133 (14). doi:10.1161/CIR.0000000000000311. ISSN 0009-7322.

